Electrocardiography
Electrocardiography
Electrocardiography, "ECG" and "EKG" redirect here. For other uses, see ECG (disambiguation) and EKG (disambiguation).
Not to be confused with other types of electrography or with echocardiography.
Use of real time monitoring of the heart in an intensive care unit in a German hospital (2015), the monitoring screen above the patient displaying an electrocardiogram and various values of parameters of the heart like heart rate and blood pressure
Electrocardiography is the process of producing an electrocardiogram (ECG or EKG[a]), a recording of the heart's electrical activity through repeated cardiac cycles.[4] It is an electrogram of the heart which is a graph of voltage versus time of the electrical activity of the heart[5] using electrodes placed on the skin. These electrodes detect the small electrical changes that are a consequence of cardiac muscle depolarization followed by repolarization during each cardiac cycle (heartbeat). Changes in the normal ECG pattern occur in numerous cardiac abnormalities, including:
· Cardiac rhythm disturbances (such as atrial fibrillation[6] and ventricular tachycardia[7]),
· Inadequate coronary artery blood flow (such as myocardial ischemia[8] and myocardial infarction[9]),
· and electrolyte disturbances, such as hypokalemia.[10]
Traditionally, "ECG" usually means a 12-lead ECG taken while lying down as discussed below. However, other devices can record the electrical activity of the heart such as a Holter monitor but also some models of smartwatch are capable of recording an ECG. ECG signals can be recorded in other contexts with other devices.
In a conventional 12-lead ECG, ten electrodes are placed on the patient's limbs and on the surface of the chest. The overall magnitude of the heart's electrical potential is then measured from twelve different angles ("leads") and is recorded over a period of time (usually ten seconds). In this way, the overall magnitude and direction of the heart's electrical depolarization is captured at each moment throughout the cardiac cycle.[11]
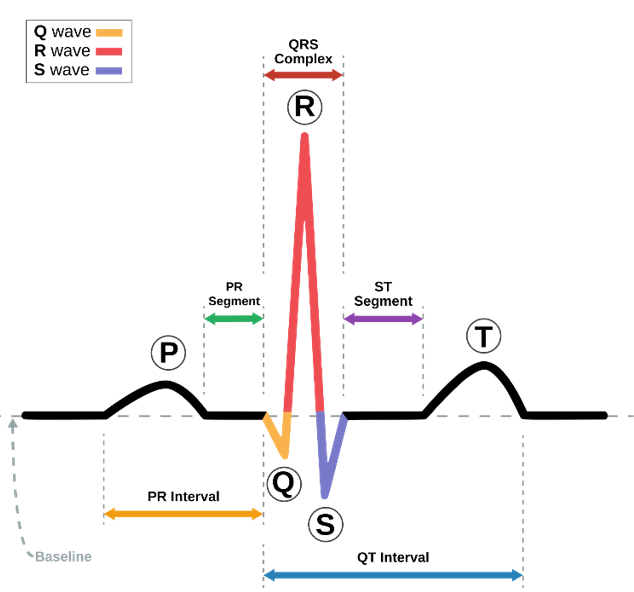
There are three main components to an ECG:[12]
1. The P wave, which represents depolarization of the atria.
2. The QRS complex, which represents depolarization of the ventricles.
3. The T wave, which represents repolarization of the ventricles.
During each heartbeat, a healthy heart has an orderly progression of depolarization that starts with pacemaker cells in the sinoatrial node, spreads throughout the atrium, and passes through the atrioventricular node down into the bundle of His and into the Purkinje fibers, spreading down and to the left throughout the ventricles.[12] This orderly pattern of depolarization gives rise to the characteristic ECG tracing. To the trained clinician, an ECG conveys a large amount of information about the structure of the heart and the function of its electrical conduction system.[13] Among other things, an ECG can be used to measure the rate and rhythm of heartbeats, the size and position of the heart chambers, the presence of any damage to the heart's muscle cells or conduction system, the effects of heart drugs, and the function of implanted pacemakers.[14]
Medical uses
A 12-lead ECG of a 26-year-old male with an incomplete right bundle branch block (RBBB)
The overall goal of performing an ECG is to obtain information about the electrical functioning of the heart. Medical uses for this information are varied and often need to be combined with knowledge of the structure of the heart and physical examination signs to be interpreted. Some indications for performing an ECG include the following:
· Chest pain or suspected myocardial infarction (heart attack), such as ST elevated myocardial infarction (STEMI)[15] or non-ST elevated myocardial infarction (NSTEMI)[16]
· Symptoms such as shortness of breath, murmurs,[17] fainting, seizures, funny turns, or arrhythmias including new onset palpitations or monitoring of known cardiac arrhythmias
· Medication monitoring (e.g., drug-induced QT prolongation, Digoxin toxicity) and management of overdose (e.g., tricyclic overdose)
· Electrolyte abnormalities, such as hyperkalaemia
· Perioperative monitoring in which any form of anaesthesia is involved (e.g., monitored anaesthesia care, general anaesthesia). This includes preoperative assessment and intraoperative and postoperative monitoring.
· Cardiac stress testing
· Computed tomography angiography (CTA) and magnetic resonance angiography (MRA) of the heart (ECG is used to "gate" the scanning so that the anatomical position of the heart is steady)
· Clinical cardiac electrophysiology, in which a catheter is inserted through the femoral vein and can have several electrodes along its length to record the direction of electrical activity from within the heart.
ECGs can be recorded as short intermittent tracings or continuous ECG monitoring. Continuous monitoring is used for critically ill patients, patients undergoing general anaesthesia,[18][17] and patients who have an infrequently occurring cardiac arrhythmia that would unlikely be seen on a conventional ten-second ECG. Continuous monitoring can be conducted by using Holter monitors, internal and external defibrillators and pacemakers, and/or biotelemetry.
